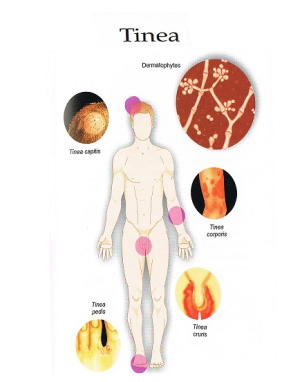
Tinea is a fungal infection of the skin. The fungi that infect the skin are called dermatophytes. The types of dermatophytes which cause tinea are epidermiphyton, trichophyton and microsporum.
Types of tinea
There are different types of tinea, named for the part of the body that is affected. These include:
- Tinea capitis – head/scalp
- Tinea barbae – beard area
- Tinea axillaris – armpit
- Tinea corporis – body
- Tinea cruris – groin (jock itch)
- Tinea pedis – foot (athlete’s foot)
- Tinea unguium – nail
The moulds that cause tinea need warmth and moisture to survive. This is why it often grows on and near skin folds, which are warm and moist due to sweating. Obesity is a predisposing factor too, as it creates more skin folds where the fungi can grow.
Signs and symptoms
Some people who have tinea have no symptoms at all. In others, some of the common signs and symptoms that are reported are:
- Itching
- Rash – the rash is red, scaly and ring-shaped
- A bad odour
- Patches of hair loss on the scalp (tinea capitis); this is because the infection targets the hair follicle
- Changes in the colour of the nail (often becomes a white or yellow colour) – tinea unguium
- Nails may also become thick and brittle
- Peeling and splitting of the skin, especially between the toes in tinea pedis
- Blisters – these are commonly further away from the area of infection and is the result of an allergic reaction to the mould
Transmission & Prevention
 This fungal infection can be spread in a couple of ways. Since tinea likes to live in hot, moist environments, communal showers, such as in swimming pools and caravan parks, are common sources of infection. Wearing thongs or sandals in these types of showers and change rooms and being careful to dry between your toes with a towel afterwards can help to prevent tinea pedis. Exposing the feet to air after drying can also be helpful, so if possible, try not to put on shoes and socks immediately after showering. Drying the armpits and other regions where there are skin folds can also help to prevent other forms of tinea. Since sweating also contributes to tinea infection, using a good antiperspirant deodorant can also help. It is also possible to contract the moulds that cause tinea from soil and young cats and dogs, so wearing gloves whilst gardening and washing your hands thoroughly after touching pets and gardening may also help protect against this infection.
This fungal infection can be spread in a couple of ways. Since tinea likes to live in hot, moist environments, communal showers, such as in swimming pools and caravan parks, are common sources of infection. Wearing thongs or sandals in these types of showers and change rooms and being careful to dry between your toes with a towel afterwards can help to prevent tinea pedis. Exposing the feet to air after drying can also be helpful, so if possible, try not to put on shoes and socks immediately after showering. Drying the armpits and other regions where there are skin folds can also help to prevent other forms of tinea. Since sweating also contributes to tinea infection, using a good antiperspirant deodorant can also help. It is also possible to contract the moulds that cause tinea from soil and young cats and dogs, so wearing gloves whilst gardening and washing your hands thoroughly after touching pets and gardening may also help protect against this infection.
If you have tinea, it is also important to try and stop spreading the infection to other members of your family or household. The infection can be spread by direct contact with others, and can also be spread via flakes of skin. After using the shower or bath, it is important to clean the area thoroughly and avoid sharing towels with others as this may also contribute to spreading the tinea infection. If you have tinea pedis, it is a good idea to wear shoes or socks inside to help prevent infected skin flakes from landing on the carpet or floor, as this is a way of easily spreading the infection to others.
Treatment
Infections of the nail can take up to 1 year to treat effectively, especially if only topical therapy is used. In severe cases, surgical removal may be indicated. Due to the hair loss, tinea capitis requires more intense therapy. Both tinea capitis and tinea unguium are treated with oral antifungal agents, such as griseofulvin, itraconazole or terbinafine. This may need to be taken for 2-3 months in the majority of cases. Oral medications can be combined with topical creams. Glucocorticoids may also be helpful as an additional therapy for tinea capitis with hair loss.
For tinea pedis, corporis and cruris, topical creams alone are usually enough to resolve the infection. Creams that are effective against fungal infections include imidazoles, triazoles and allylamines. These should be applied 2 times per day, and continue to be applied for 1-2 weeks after the infection has resolved to limit the chance of a recurrence. If the tinea does not resolve with topical therapy only, an oral antifungal agent may also be added.
Tinea can sometimes be difficult to identify. Dermatologists are highly experienced in managing this condition. If you have any questions or concerns about your skin, contact our clinic for an appointment. Contact us today.



